Using technology to advance our care
In line with EMHS’ vision of healthy people, amazing care, EMHS continues to progress the digital strategy — smart EMHS — and other digital initiatives to achieve our digital future state:
You connect with us, when and how you want to. We connect with you, when and how you need us.
A snapshot of just some of these initiatives is provided below:
Office of the Auditor General – General Computer Controls audit
EMHS participated in its second General Computer Controls (GCC) audit, which has resulted in a reduction from 18 open findings in 2021 to 11 open findings in 2022.
In the 12 months between audits, EMHS was able to close nine, and downgrade the severity of two of the 2021 findings — with two new findings identified. The qualification and significant findings relating to segregation of network and unauthorised device connectivity remain this year, and are being addressed through participation in the whole-of-health Critical ICT Infrastructure Program.
Registration of Rapid Antigen Test (RAT) results
EMHS has initiated a web-based application to register RAT results for patients being triaged in ED. This allows ED consultants and wards to see near real time views of the results of patients in the ED.
Transition to Microsoft (MS) Power BI
In 2021-22, EMHS progressed plans to transition to Power BI (business intelligence tool), which will bring innovation and integration opportunities, enabling users to perform data preparation and discovery and share insights in a single solution. The move to Power BI in early 2022-23 will improve integration with existing Microsoft products, including:
- easy sharing of content, including on MS Teams and SharePoint
- improved mobility with secure access to reporting and analytical content from inside or outside WA Health.
Staff Absence Management Process
Maintaining service delivery amid severe staff shortages has been a universal challenge for healthcare services throughout the pandemic.
An innovative dashboard, launched in February 2022, proved an invaluable tool for EMHS in maintaining oversight of staffing. The dashboard was part of a Staff Absence Management Process (SAMP) that was developed in-house by our award-winning DDI team in collaboration with our people and capability and clinical services teams. The SAMP has two components — a web-based furlough declaration form and staff absence management dashboard.
Staff unable to work due to COVID-related reasons or personal/sick leave complete a declaration form prior to the start of their shift. The dashboard extracts data from these forms to create a real-time snapshot of staff absences across EMHS by site, occupational group and area/department. Information in the dashboard is updated every 15 minutes and is used to coordinate staff and manage demand/critical services. This enables EMHS to identify and respond quickly to areas of staffing need.
RPBG Deputy Director of Clinical Services Dr Sumit Sinha-Roy said: “It enabled the RPBG medical workforce team that I manage, to pre-emptively (or really speedily), with collaboration from other clinical Heads of Departments, move junior doctors across services to supply clinical teams that were short-staffed, to maintain their services.”
Valentine’s Day marks the start of Wi-Fi milestone
Keeping in touch with loved ones became easier for EMHS patients who found themselves in hospital on Valentine’s Day 2022.
That’s because 14 February was the day patients joined staff in being able to access free Wi-Fi, fulfilling the final milestone in the EMHS’ Digital Infrastructure Enablement (EDIE) Wi-Fi project.
The Wi-Fi project — that made EMHS sites Wi-Fi hotspots — was a massive undertaking and its completion was a major achievement.
Putting Wi-Fi into sites after they were built — especially ones that were built before electricity was standard — was a challenging experience.
The provision of Wi-Fi to patients enables them to stay connected to loved ones and communities, helping them feel more comfortable while in hospital.
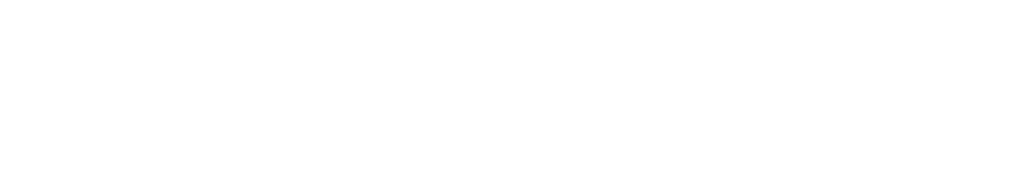
Ambulatory video electroencephalographic monitoring
An accurate diagnosis of epilepsy and similar conditions is essential for safe and high-quality patient care. Inpatient video electroencephalographic monitoring (vEEG) is the gold standard for diagnosis, but requires hospitalisation, is expensive and is inconvenient
for patients.
The pandemic prompted EMHS to consider approaches other than traditional inpatient care. Home-based Ambulatory vEEG monitoring (AVEM) was trialled as an alternative option because it replicates inpatient vEEG monitoring, is less expensive and is more accessible for patients.
During the reporting period, EMHS’ Innovation Hub piloted an AVEM program at RPH. The pilot, led by Consultant Neurologists Dr Jacqui-Lyn Saw, Dr Nicholas Lawn and Professor John Dunne, has to date enrolled eight patients with unexplained paroxysmal neurological symptoms, requiring prolonged EEG monitoring. AVEM was able to clarify symptoms and inform clinical management in six of eight patients, a proportion comparable to that obtained with vEEG.
This preliminary data indicates that home-based AVEM has the potential to transform the investigation and management of patients with paroxysmal neurological symptoms, with lower costs and improved patient convenience.

Information technology given end-user focus
As part of the EMHS Digital Strategy, improving the end-user computing (EUC) experience for staff and patients continued to be an important focus for EMHS during the reporting period.
As part of its EUC program, EMHS has been working on initiatives that will not only make accessing and navigating applications easier, but also possible from anywhere, at any time and from one or more devices.
Workstation on Wheels (WoW) and Desktop Device Refresh were two initiatives of the EUC program that made a real difference to EMHS activity in 2021-22.
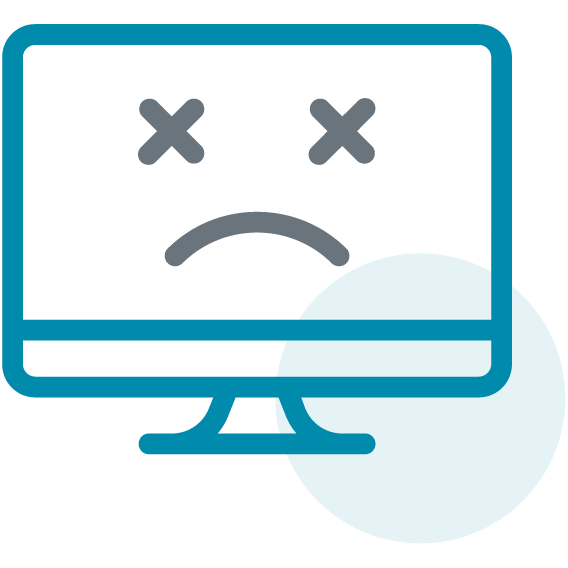
Complete digital workspace failure by volume
WoW is a practical initiative that has enhanced the delivery of care on our wards. Doctors, for example, without having to leave the patient’s bedside, are able to look up results in real time, or discuss x-ray results more easily.
At KH, WoWs have enabled social workers and patients to attend National Disability Insurance Scheme (NDIS) meetings together from the patients’ bedside.
The Desktop Device Refresh involved the replacement of more than 1000 desktop and laptop computers, most of which were more than seven years old and running outdated software.
The newer devices and applications have improved workflow and security by providing staff with access to virtual desktops (which enabled them to work from home) while products such as MS Teams enabled them to collaborate safely during the COVID-19 emergency. Enhanced authentication features also reduced the risk of non-authorised access to restricted information.

Virtual getaways prove treat for patients
Palliative care patients at KH got the chance to escape their hospital rooms for a while — without needing to move an inch.
As part of a virtual reality (VR) trial exploring how VR technology could improve quality of life, the patients donned special headsets, where they had the chance to travel back to their hometowns or tick off bucket list items and final wishes.
The project’s lead, Senior Occupational Therapist Karina Bowden, learnt of the technology at a conference, where the idea was promoted as an innovative way to increase patients’ quality of life while in hospital.
Feedback from the patients was positive with all saying how nice it was to escape from their rooms and experience the natural world for a while.
“Globally there isn’t much research about the benefit it could have for patients, but we’ve seen it successfully used in places like the United Kingdom during COVID as a way for patients to connect with and see their loved ones,” Karina said.